
Heath loves team sports: baseball, basketball, football, you name it. The Tuttle family cherishes the support of a large team of family and friends in the good, fun times and in the hard times.
This site is to keep the beloved members of this team informed about the latest with our favorite all-star.
Wednesday, September 8 — A busy week and next steps
/34 Comments/in ht /by Carrie TuttleOn Tuesday we had walked from the PET scan in the Duke Cancer Center back to the 4th floor of the CHC (Children’s Health Center) with the PET IV still in, hoping that they could use his IV to draw labs. As we were telling the story of our “journey” to the nurse drawing labs (the IV worked!), I said off-hand, “Heath has been such a good sport in the midst of all of this…” He turned and looked at me, with that Heath half-smirk, and said, “Do I really have any other option?”
And there he is. His whole life with so many medical challenges.
That is what finally brought me to tears last night. We would switch places with him in a minute, but we can’t. All we can do is love him and care for him. Any of you who have cared for a loved one who is suffering knows this feeling deep in your soul.
The PET scan results were not what we had been hoping for. Not enough progress had been made. So, it is now on to the next steps. The oncology team, in conjunction with cardiology and nephrology (those darn creatinine numbers…grrrr…) are in the process of making decisions about the cocktail of drugs, but we know we’ve got to hit this with the harder stuff. They had been hoping to get the general surgery team to put in a port during his heart catheterization tomorrow, but alas, we just found out that it is too tricky to navigate different procedures in different spaces (cath lab instead of OR.) So, they’ll put a port in on Friday. And then will keep him inpatient for several days with the intention to begin the next round of chemo with the new drugs on Saturday. Apparently, there is much more monitoring that needs to take place with any of the options. That is all we know right now. We should have a better understanding tomorrow.
Because he had been feeling pretty good, I think we all thought we’d get the news that we wanted (much more progress on that mass; that he could keep on with the least harsh treatment.) But alas, we always knew this next way was more probable. But we felt the sting of disappointment last night.
Again, the roller coaster keeps going.
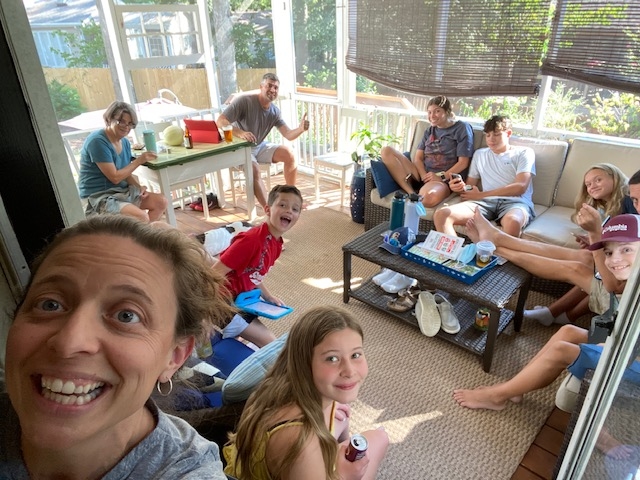
We cling to glimpses of “normal.” When the team told us that they thought we had a couple of weeks of “less sick/less immune-suppressed,” Pete and Melinda (my brother and sister-in-law) and the kids came to visit from Virginia. They stayed at Mom and Strow’s outside Chapel Hill and all who weren’t our immediate 5 masked inside (that is what Hemonc has asked us to do for now), of course. But we had the gift of some hangout time with the cousins. We knew it wasn’t totally “normal,” but listening to the banter, the laughter, the fantasy football drafting throughout the weekend, well, that was spirit-lifting and filling. It is a reminder of why you keep fighting when you feel really crummy.
So now we keep going; he keeps going, a better sport than any of us adults can imagine being, frankly. We know, Heath knows, that we don’t do this alone. We are grateful for the glimpses of “normal” and the glimpses of grace along the way, and we most certainly feel your love and prayers.



Friday, September 3 — First course complete!
/31 Comments/in ht /by Chris TuttleSo…..Carrie and I learned last weekend (when we posted a positive update and then spent the overnight hours in a rough patch), not to do updates too late in the day! As evening comes the anxiety rises a bit.
Thankfully, it has been a good two days. Tuesday was a long clinic day with labs, and some concern about dehydration – so we plugged up IV fluids for a bit. He was sick overnight Tuesday night/Wednesday morning, so we visited our clinic friends on Wednesday as well, though only for a few hours. The kind woman on Thursday who did the entrance covid screening looked at Heath and said, “I did this for you yesterday, didn’t I?”
Thursday’s infusion was as smooth as those things could be. We had a wonderful hour with a dear friend who works for the Hospital School (yes, that is a thing), and who is working with Heath’s Lakewood teachers to make a plan for his education this fall. They started working on a book to read and a project to be working on. It was exciting to see some of this beginning, but it came to an abrupt conclusion when they started his pre-infusion meds, especially the Benadryl. Heath slept through the first two hours of his infusion – which, like last time, took 3.5 hours. He didn’t feel too nauseous and even had a snack near the end. It was a long day, but the beautiful weather meant he could come and lay down on the porch, or inside. He ate a normal dinner as the rest of us went back and forth from a Jordan tennis match for Ella Brooks, and worked to stay hydrated. Keeping him eating and drinking with the illness and accompanying weight loss is a constant challenge, especially when you get sick pretty regularly. But we are getting creative with protein drinks, and Carrie even found some chocolate chip cookies with protein at Target (everything is at Target, right?!), which are a hit. You can imagine it, can’t you? “Dad, I’m having another protein cookie! Look, it’s good for me!”
Thursday was a good night of sleep for all, and has been a slower day for Heath to rest, as Wilson and Ella Brooks went to school. As I rush out to battle the Jordan pickup car line for the first time (Yikes!), I wanted to share one more thing we’ve been thinking about a lot. Most of us are trained, as we grow and learn, to try and think about the big picture. Where are things moving? How can we plan accordingly? In organizations, we ask questions about long-term vision – who are we called to be? Then we can align priorities and work with the vision. We try to organize teams and think sequentially: THIS will happen, then THIS, then THIS. But we have, thus far, found that kind of thinking profoundly frustrating. This disease is something you can’t plan for or work around. Our significant problem-solving skills are inadequate. Carrie and I work hard to function at a high level and keep the trains moving and knock things off of the list. None of these skills can help us now. Each day brings its own set of challenges that are very difficult to plan for. And if we do plan, we are only frustrated. We’ve had to work to bring our vision down to ground level. What will we do today? How does he feel this morning? Certainly, as this goes on, we learn the rhythms of the clinic better and memorize the names of the medications. That is already helping us. But trying to look beyond that is a recipe for disaster because you’re always measuring where you are and how anyone is doing against your expectations, which is a trap. So, we’ll be grateful for a beautiful afternoon and a protein cookie. We’ll be grateful for the friends who will bring dinner this evening. We’ll be grateful for the neighborhood happy hour that happens every Friday at 5 right in front of our house, instituted in the pandemic. And maybe we’ll all walk the dog together in the cool of the evening. And for today, we pray, that will be more than enough. We are so grateful for all of you.
Tuesday, August 31 – No infusion today!
/19 Comments/in ht /by Carrie TuttleIf we have learned a few things during our almost 13 years navigating the medical system, mostly here at Duke but I suspect it is the same everywhere, you live into “hurry up and wait” hospital time as well as just knowing that schedules and plans change for all sorts of reasons. We are grateful for the loving care and big brains who have saved countless lives, including our son’s, so we learn to have patience and know that things change from moment to moment in a hospital setting.
Heath and Chris had a HemOnc clinic visit, labs, and an echo (we do this each time to check his heart) this morning, but he is going to go back for his 3rd infusion at the Valvano Day Hospital on Thursday. It seems that this particular change is just based on staffing (more on this further down). Other than being annoyed at having to get up early multiple days, Heath was feeling good this morning.
Chris and I often “laugh” about some rolling lists that we have in our life:
- “They didn’t teach us THAT in seminary…”,
- “THAT needs to go on the premarital counseling list…”
- “NO ONE told me about THIS part of parenting…”
- and in the midst of this medical crisis, we are adding more to the “Medical information that I wish I didn’t have any reason to know.”
On that last list, this week we add to it some information that pertains to our schedule for next week. Since this week marks the end of the first three-week round, next week will be all about testing: Abdominal imaging to look at the impact of the first three infusions and the regular semi-annual heart tests that were postponed from when they were originally planned in early August (imaging, catheterization, and labs.) This week we learned that you can’t do a heart catheterization w/ coronaries (contrast/dye used) and PET scan and CT scan all on the same day. The contrast/dye that they use in all these scans has dextrose in it. PET scans need to have no contrast (dextrose) until right before you do the scan so you can “light up” the right spots. But you have to do heart cath NPO as well and also with contrast. CT scan also uses contrast. AND, contrast can also be hard for your kidneys to “get rid of.” So, alas, all of that is to say that Heath will have scans one day next week (probably Tuesday, Sept 7) and his heart catheterization early Thursday morning, Sept 9 instead of all in one visit as we hoped.
I suspect we’ll keep adding to that glorious list.
So, back to hospital staffing.
I got teary last night when I heard the news story of a US veteran who died from complications of gall bladder issues because hospitals were over-run and doctors were having to “play musical chairs” with care.
On Saturday night, right after I posted the last update, Heath got sick again. Heath said, “am I going to have to go back to the hospital?” and I said, “buddy, we’re going to do everything we can not to have to head to the crowded ED with all the COVID numbers rising.” (Obviously, we didn’t and thanks to a great medical team and a really kind pharmacist at Walgreens at 2:30 a.m., we have a nice stash of Zofran now.)
I know that people say that not getting vaccinated or even just not wearing a mask is their personal choice. But I would like to remind you that full hospitals and nursing shortages make it more difficult for OTHERS to get treatment for all sorts of other ailments–whether that be a cancer treatment or emergency gall bladder surgery.
I am not sure that that is exactly why Heath is not having an infusion this morning, but it was a good reminder to me of the way that burnout and shortages in staff affect all of us.


